Hypermobility and Pelvic Girdle Pain in Pregnancy
Pregnancy is a time of incredible change for a woman's body. Along the journey of physical and hormonal shifts, one common issue that many expectant mothers face is pelvic girdle pain (PGP). This may look slightly differently for those who have pre-existing hypermobility (increased joint flexibility).
What is Pelvic Girdle Pain?
Image sourced from bodyorganics.com.au
PGP is characterised by pain in the pelvic region which may present around the hips, at the pubic bone/groin area or lower back; and the pain may radiate down the legs. It typically arises from dysfunction or irritation of the joints that form the pelvic girdle: the sacroiliac joints (where the low spine meets the pelvis) and the pubic symphysis (the joint at the centre of the front of the pelvis).
Common symptoms of PGP can be (but are not limited to): pain with getting in and out of bed or the car, pain rolling in bed and pain standing on one leg (for example, while putting on pants or shoes and socks while standing on one leg). PGP is most common during pregnancy, due to the hormonal changes, change in weight distribution impacting the body's centre of gravity and resultant changes in biomechanics.
Hypermobility and Its Impact on Pelvic Girdle Pain
Hypermobility is a condition of increased flexibility at the joints of the body. This is due to the connective tissue (i.e. the ligaments and tissues around the joints) being more flexible than usual. While some degree of hypermobility can be completely normal, for others, it can lead to joint instability and an increased risk of pain and discomfort. Pre-existing hypermobility can mean the increased joint mobility in pregnancy is even more pronounced. Recent studies show that women with hypermobility are more likely to experience PGP in the first trimester than women who do not have hypermobility.
For women with hypermobility, the added laxity in the ligaments and joints can put increased strain on the pelvic girdle. Here’s how:
Increased Joint Instability: Hypermobility leads to more flexible ligaments, which can cause the pelvic joints to be less stable. During pregnancy, the hormones oestrogen and relaxin promote connective tissue laxity to allow the body to prepare for childbirth. While this is necessary for labour, for someone with pre-existing joint laxity, the combination of hypermobility and increased oestrogen and relaxin can cause excessive joint movement, leading to discomfort or pain in the pelvis.
Altered Posture and Movement Patterns: Women with hypermobility may have a tendency to adopt compensatory movement patterns to avoid pain in their joints. This can put additional strain on the pelvic girdle, particularly during pregnancy when changes in posture occur naturally due to the growing belly. Over time, these altered patterns can result in chronic pain and discomfort.
Increased Pressure on the Pelvis: The added weight and shifting centre of gravity during pregnancy increases the load on the pelvic joints. In hypermobile women, the body may struggle to provide enough support to the pelvis, increasing the likelihood of developing pelvic girdle pain.
Fatigue of Stabilising Muscles: The stabilising muscles of the pelvis, such as the glutes, core, and pelvic floor muscles, play an important role in maintaining joint stability. Women with hypermobility may have underactive or weakened stabilising muscles, which can further compromise pelvic joint integrity during pregnancy. This lack of support may contribute to the development of PGP.
Compensatory Muscle Tightness: When hypermobility is present at joints in the body, often the surrounding muscles may increase their tone to compensate for the excess movement present. With the hormonal changes of pregnancy on top of already-flexible hypermobile joints, increased muscle tightness can occur, which can then further contribute to the discomfort of PGP.
Identifying Hypermobility
While hypermobility may not always be immediately obvious, there are some simple assessments that help clarify whether it is present in an individual.
Answering yes to 2 or more of the following questions suggests hypermobility:
Can you now [or could you ever] place your hands flat on the floor without bending your knees?
Can you now [or could you ever] bend your thumb to touch your forearm?
As a child, did you amuse your friends by contorting your body into strange shapes or could you do the splits?
As a child or teenager, did your kneecap or shoulder dislocate on more than one occasion?
Do you consider yourself “double-jointed”?
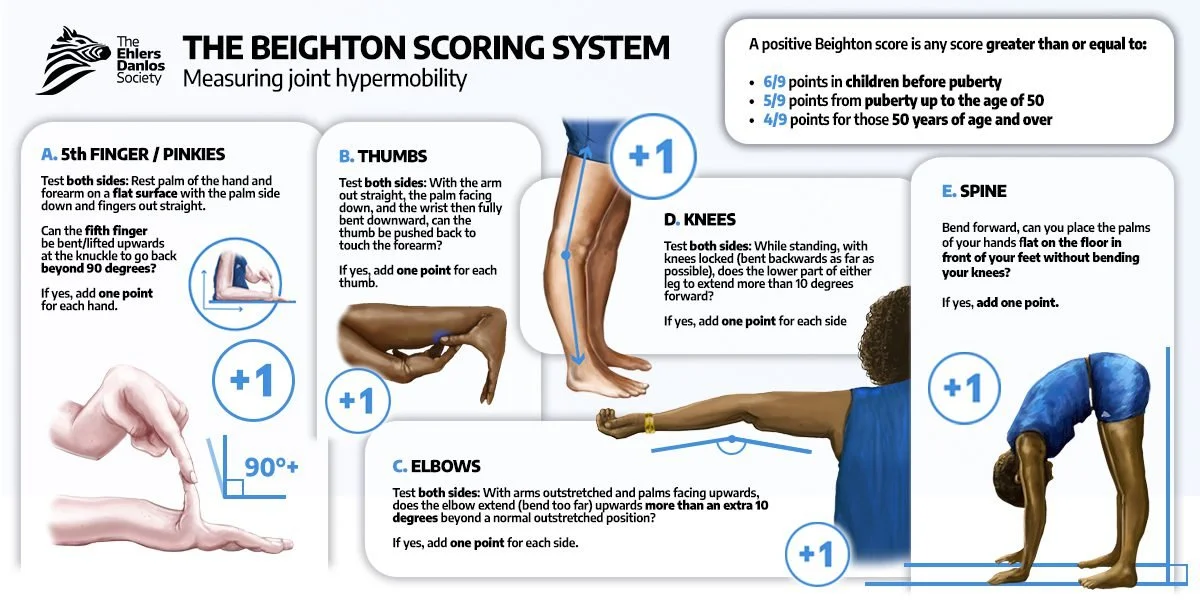
Physiotherapists can also assess joint hypermobility using the Beighton Scoring System, which assesses various joints in the body.
If you suspect hypermobility is contributing to your pelvic pain during pregnancy, it’s important to seek an assessment from a qualified pelvic health physiotherapist. They can provide a comprehensive evaluation of your joints, movement patterns, and posture to determine how hypermobility may be affecting your pelvic health.
Managing Hypermobility-Related Pelvic Girdle Pain in Pregnancy
Fortunately, there are various strategies to manage, reduce and even prevent pelvic girdle pain in pregnancy, especially for those with hypermobility. Here are a few tips that can help:
Early Prevention: Presenting to physiotherapy prior to conception for assessment of hypermobility, muscle tightness, strength and motor control can allow a physio to provide you with a tailored program to prepare your body for the changes of pregnancy. They can also give you tips and tricks for managing any aches or pains that may arise so you can get on top of them straight away if they do occur!
Pelvic Health Physiotherapy: Working with a pelvic health physiotherapist during pregnancy is one of the most effective ways to manage pelvic girdle pain. They can teach you how to activate and strengthen the muscles around your pelvis, including the pelvic floor, core, and glute muscles, which will provide additional stability to your joints.
Postural Awareness and Education: Proper posture and body mechanics during daily activities can make a significant difference in managing pelvic pain. A physiotherapist can teach you how to adjust your posture, sit, stand, and move in ways that reduce strain on the pelvic region.
Pelvic Girdle Pain Exercises: Gentle, targeted exercises can help to stabilise the pelvis and reduce pain. These exercises are typically designed to strengthen the muscles around the pelvis while improving mobility and flexibility where needed. The key is to ensure that exercises are adapted to your unique needs, as over-stretching can aggravate symptoms in hypermobile individuals.
Supportive Devices: Using a pelvic belt or maternity support band can help provide external support to the pelvis, reducing joint instability. A physiotherapist can guide you on how to wear these devices correctly to get the most benefit and which one is best suited to your needs.
Activity Modification: Modifying high-impact activities or movements that involve sudden or excessive twisting, bending, or lifting can help prevent further strain on the pelvic region. Your physiotherapist can suggest alternative ways to stay active while avoiding exacerbation of symptoms. Even simple changes to how you get in and out of the car or roll in bed can make a significant change to your pain.
Mindful Movement: Yoga, swimming, and other low-impact exercises can be beneficial for improving flexibility and strengthening the muscles around the pelvis. However, it’s essential to practice mindful movement to avoid overstretching or putting too much strain on the joints.
Conclusion
Hypermobility can increase the likelihood of experiencing pelvic girdle pain during pregnancy, but with the right approach, many women can effectively manage and reduce discomfort. By working with a pelvic health physiotherapist to address joint instability, strengthen the pelvic muscles, and modify movement patterns, you can navigate pregnancy with greater ease and comfort.
If you are pregnant and dealing with pelvic pain, consider reaching out to a pelvic health physiotherapist for personalised advice and support. With the right tools and strategies, you don’t have to let hypermobility or pelvic girdle pain define your pregnancy experience. If trying to conceive is part of your plan for 2025, set yourself up for the best possible journey by seeing us beforehand to prevent onset altogether where possible.
Written by Amy Duerkop, Pelvic Health Physiotherapist.